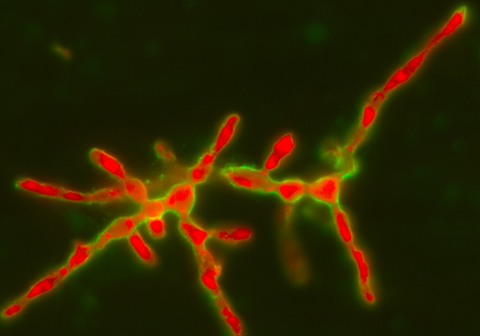
The UPV/EHU's Fungal and Bacterial Biomics research group has established the existence of a new, hitherto unknown resistance mechanism in the fungus Lomentospora prolificans (L. prolificans). This microorganism is multiresistant to the currently used antifungal drugs (antibiotics developed to combat fungi) and leads to between 80% and 100% mortality in patients with weakened immune systems. This study will therefore enable more effective drugs to combat this fungus to be designed.
A resistance mechanism is discovered in a fungus capable of causing 90% mortality
The study by the Fungal and Bacterial Biomics research group of the UPV/EHU-University of the Basque Country has been published in the PLOS ONE journal
First publication date: 09/06/2017
The research was led by the lecturers Fernando L. Hernando, Aitor Rementeria and Andoni Ramirez and had the participation of the researchers Aize Pellón (whose PhD thesis prompted this piece of work), Idoia Buldain, Xabier Guruceaga, and Aitziber Antoran. Entitled "Molecular and cellular responses of the pathogenic fungus Lomentospora prolificans to the antifungal drug voriconazole", it has been published in the leading PLOS ONE journal.
The microorganism L. prolificans (previously known as Scedosporium prolificans) is a filamentous fungus belonging to the group commonly known as moulds, some of which can be seen growing on rotting food (fruit, bread, etc.). And they are distinct from single-celled yeasts, such as Candida albicans or Saccharomyces cerevisiae, which are significant in clinical practice and in the food industry, respectively. The fungus L. prolificans is also common and fairly routinely found in city soils and on industrial estates. Contact with it does not usually cause ailments in healthy individuals thanks to their immunological systems.
However, as Andoni Ramirez, one of the authors of the article, explained, it causes "very serious infections" in patients with an underlying disease such as "cystic fibrosis" or with "weakened immunological systems", as in the case of patients undergoing chemotherapy to treat some kind of cancer, patients who have undergone an organ transplant, or who are suffering Acquired Immune Deficiency Syndrome (AIDS) due to HIV.
This fungus, according to the research, displays great resistance to the most common antifungal drugs such as voriconazol, which is one of the "drugs of choice for treating" infections caused by filamentous fungi. "This work is hugely significant because it establishes the existence of a new resistance mechanism that has so far remained unknown in fungi. We spotted a significant change in the cell wall in response to the antifungal drug voriconazol, which is used preferentially to combat this fungus and other fungal species. These changes take place in the size and composition of its cell wall," he explained.
New therapeutic strategies
So this work constitutes the first description of these responses as a defence mechanism against an antifungal drug, thus opening up a new field of possibilities with a view to designing new molecules that will enable this and other fungal infections to be treated more effectively. "Unlike what happens with antibacterial agents, the variety of antifungal compounds is very limited and they function with few mechanisms for acting differently. So should resistant strains or species emerge, the options available to hospitals often tend to be very limited. So the discovery of new resistance mechanisms could firstly increase the number of targets for directing drugs towards; and secondly, explain the intrinsic as well as acquired resistance in other species of pathogenic fungi," he pointed out.
For the time being, the research being done by the UPV/EHU's Fungal and Bacterial Biomics research group is basic, in other words, it is generating the knowledge needed so that new therapies can be designed in the future. "In this respect, the next aim is to identify the enzymes needed for the changes that the fungus L. prolificans carries out in its wall in response to the antifungal drug and also to study them and come up with new therapeutic strategies".
Although it is necessary to bear in mind that in any area of biomedicine the move from the lab to the patient is long (several years) and difficult owing to the sheer quantity of tests that have to be conducted. "What is more, as happens with the so-called rare diseases, the infections caused by fungi of this type have a low incidence in the population and therefore, despite the high mortality they pose, it is difficult that there will be organisations interested in investing in research into them. That is why progress is always more problematic and slower," pointed out Ramírez.
Bibliographic reference
- Molecular and cellular responses of the pathogenic fungus Lomentospora prolificans to the antifungal drug voriconazole.
- PLOS ONE (2017)
- DOI: 10.1371/journal.pone.0174885