An in-house clinical practice manual for dealing with patients with community-acquired pneumonia who are referred to the healthcare services was introduced in 2001. It has since been used to create a prediction rule for the patients' outcomes, and now a piece of research defended at the UPV/EHU and conducted at the Galdakao-Usansolo and Inner Area Hospital (OSI Barrualde) proposes that certain biomarkers also be analysed so that those patients likely to have a poor outcome can be identified more accurately.
The spotting of pneumonia patients likely to have a poor outcome is improved
A study presented at the UPV/EHU-University of the Basque Country shows that including biomarkers in the routine prediction rules improves the results
First publication date: 14/12/2016
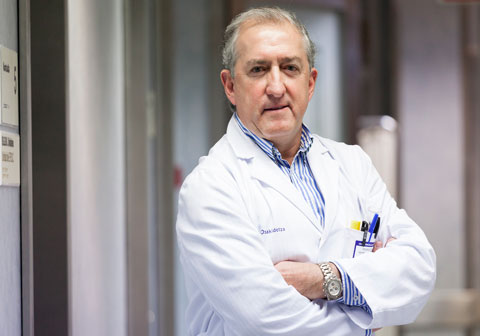
Community-acquired pneumonia, in other words, that which is not caught in a hospital environment, is a major cause of morbidity and mortality with a rate ranging between about 2 and 8 cases for every 1,000 inhabitants per year; it results in a mortality rate of between 10% and 15% in those patients requiring admission to hospital, and this rate is even higher for those requiring admission to an intensive care unit (ICU). All this "means a huge burden on healthcare systems in terms of visits to the primary healthcare doctor and A&E services, hospital admissions, medical treatments and follow-up care", explained Pedro Pablo España, the head of Pulmonology at Galdakao-Usansolo Hospital and author of the study submitted at the UPV/EHU.
"To prevent the most severe complications, it is necessary to know how to assess during the diagnosis how serious the pneumonia is likely to be because it is very important to treat it early". On this basis, various protocols were implemented and developed to assess and classify the patients with pneumonia. In 2001 they introduced a clinical practice manual designed to standardize the action of healthcare staff and prevent variability in the care that existed. "This constituted an improvement in the results and allowed us to store information on the patients treated".
In addition, they began to use scales to predict seriousness based on the universally used mortality prediction. These scales, based on certain physiological variables, such as blood pressure, the amount of oxygen in the blood, analyses or X-ray images, enable the patients with greater need for monitoring and more aggressive treatment to be identified.
The data that were gathered through the introduction of the clinical practice manual nevertheless allowed an in-house predictive rule to be developed and implemented in 2006, and which is known as the SCAP score. "After it had been validated at various hospitals, we were able to confirm that it offered results that were considerably better than the rules used previously", explained the Pulmonologist.
Biomarkers to provide additional information
Yet given the fact that the new rule had certain limitations, "the study of various serum biomarkers was considered to be of interest in order to identify the patients who used to be categorized as low-risk ones but whose outcomes were poor in the end, as well as those patients categorized as high-risk ones but who progressed favourably. We began to think that the immunological system of each patient reacts differently when dealing with the same condition, so we considered analysing some markers of the host response to inflammation. When faced with any infection, the immune system defends itself by producing inflammation to try to contain the infection. But if that response is exaggerated, the prognosis tends to be worse," he pointed out.
As Dr España explained, he has been able to show that "by analysing certain biomarkers, above all procalcitonin (PCT) and proadrenomedullin (Pro-ADM), which provided the best result, and associating them with the already known prediction rules, the predictive power of the rule was improved. In other words, it provided us with even more information in specific cases. Above all, in patients displaying a low risk but having a high biomarker, we are alerted that something could go wrong and this enables us to make a more suitable choice as to treatment and place of care".
Additional information
Pedro Pablo España-Yandiola (Bilbao, 1958) is the head of Pulmonology at Galdakao-Usansolo Hospital. This study was part of his PhD thesis read at the UPV/EHU's faculty of Medicine. It was possible to conduct the processes to validate and compare the rules developed at many hospitals thanks to the close collaboration with the various health centres of Osakidetza (Basque Autonomous Community Public Health Service) and participation in multi-centre studies on a national level.
Photo: UPV/EHU